Monica Pia P. Reyes
St. Luke’s Medical Center Global City, Philippines
Title: Cytomegalovirus-Varicella Zoster Meningoencephalitis and Ischemic Stroke in an HIV-AIDS patient: a Case Report
Biography
Biography: Monica Pia P. Reyes
Abstract
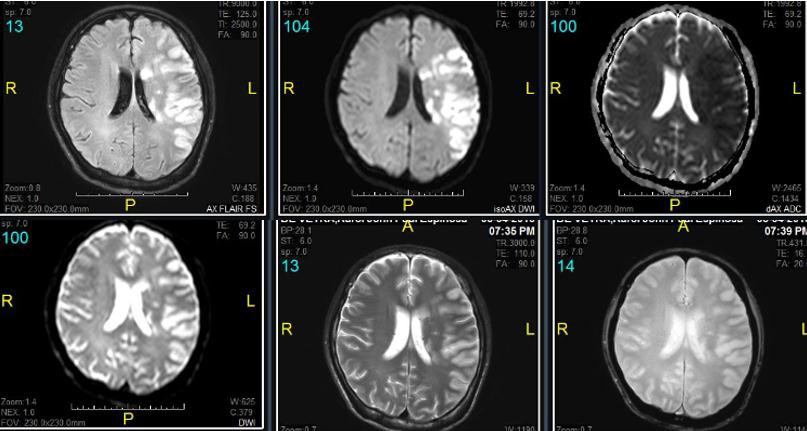
Along with the increasing number of newly diagnosed Human Immunodeficiency Virus (HIV) patients per day in the Philippines (26 new cases/day)1 is an increasing number of HIV patients diagnosed with Central Nervous System Infection (CNSI) and Stroke. A study shows that the risk of ischemic stroke was higher among those with HIV infection compared with uninfected people (hazard ratio 1.17)2. Mechanisms of ischemic stroke include HIV-associated vasculopathy, opportunistic infections or neoplasia, cardioembolism and coagulopathy3. This case report aims to present a CNS co- infection of the three most documented viruses that causes stroke: Cytomegalovirus (CMV), Varicella Zoster Virus (VZV) and HIV. The inflammatory cascade in these infections promotes atherosclerosis, plaque rupture, and thrombosis, leading to ischaemic stroke4. A 35-year-old male with HIV who is non- compliant with anti-retroviral therapy and who had recent untreated Shingles was brought in with decreased sensorium, signs of meningeal irritation and right-sided neurologic deficit. Computed Tomography scan revealed cute to Subacute Infarct, Left Middle Cerebral Artery Territory (Figure 1). He was admitted and started empirically on Vancomycin, Ampicillin, Cefepime and Ganciclovir for Central Nervous System Infection. HIV work-up revealed a CD4 of 11 cells/mm3 and HIV-1 RNA of 1,124,215 copies/mL. CMV IgG is positive at 65 U/mL. Lumbar tap done had an elevated opening pressure with elevated cerebrospinal fluid (CSF) protein, low- normal CSF glucose, and pleiocytosis with lymphocytic predominance. Viral panel showed CMV viral load of 634,000 copies/mL and VZV IgG 44.4mIU/L clinching the diagnosis of concomitant CMV-VZV meningoencephalitis in this HIV patient. Magnetic Resonance Imaging and Angiogram is compatible with viral vasculopathy (Figure 2). The pathogenic mechanisms of VZV reactivation in the CNS include neuronal and glial direct infection and immune-mediated lesions including vasculitis and demyelinization5 while CMV infection of vascular smooth muscle cells induces production of powerful pro-inflammatory cytokines which accelerate atherosclerosis development6. This might be the first reported case of co-infection of the CMV- VZV-HIV meningoencephalitis and Ischemic Stroke.