Day 2 :
Keynote Forum
Reza Nejat
Bazarganan Hospital, IRAN
Keynote: IVIG in Sepsis: Review article and case report of three critically ill patients with sepsis discharged in health

Biography:
Dr. Reza Nejat is a board certified Anesthesiologist, FCCM and ECFMG certified. He was graduated from Tehran University of Medical Sciences (TUMS) as a GP and achieved his expertise in Anesthesiology from Iran University of Medical Sciences. Fellowship in Critical Care Medicine at Sina Hospital, TUMS, made him fascinated to molecular medicine with inclination to sepsis and acute heart failure. IVIg has been one of his field of interests and experience for the past 4 years.
In addition to his positions as the chief of few hospitals and as an associate professor in Shahid Beheshti University of Medical Sciences for 8 years, he has 4 published books in the fields of cardiology, nephrology, fluid and electrolyte, nutrition, metabolism and endocrinology. He has established his website on which he publishes his articles. Dr. Nejat has presented a few articles in different conferences.
Abstract:
Statement of the problem: Intravenous immunoglobulins (IVIG) contains immunoglobulins pooled from the plasma of 3000 to 10000 individual blood-donors. This preparation was developed originally in 1952 as a therapeutic milestone in primary hypo-gamma-globulinemia. IVIG has subsequently been proved to have therapeutic efficacy for an ever-growing number of conditions in diverse fields of medicine. Presuming the protective characteristic of its pluripotent antibody content, IVIg is expected to have explicit impact in sepsis, yet FDA has not approved and Surviving Sepsis Campaign Guidelines (SSCG) 2012 discouraged its administration in adult sepsis.
Methodology: By reviewing of relevant articles searched through internet from 1990 to 2016, the efficacy of IVIg as an adjuvant treatment in improving the outcome in systemic inflammatory response syndrome (SIRS) and sepsis was surveyed. Based on the literature it is discernible that SIRS and sepsis with high rate of mortality in ICUs are actually detrimental much more owing to dysregulated immune system responses overwhelmed by disarray of cytokines and chemokines, declining of endogenous immunoglobulins and even deranged activation or suppression of relevant gene domains. According to the latest definition of sepsis in 2016, this dysregulated host response to infection renders the scene toward organ dysfunction.
IVIg was given to three highly critically ill patients of 95, 37 and 11 years of age, with severe sepsis due to iatrogenic sigmoid perforation, post-ERCP necrotizing pancreatitis and severe multiple trauma following collision with a truck, respectively. Before administration of IVIg the patients was given intensive care with administration of appropriate antibiotics and keeping the energy, fluid and electrolytes in a balance mode. They all recovered from sepsis and were discharged in good health.
Conclusion: Based on this review article and case report, immune-modulatory characteristic of IVIG may restore the pathobiological host responses to normal and improve the outcome in sepsis.
Keynote Forum
Ali karami
Baqiyatallah University of Medical Sciences,Iran
Keynote: The role of microbiology laboratories and specialists in passive defense against biological threats

Biography:
Ali Karami is Molecular biologist, Medical Biotechnologist and expert in Genetic Engineering working on Molecular detection of infectious diseases, cloning, expression and purification and characterization of recombinant proteins for medical applications. I also have been working for long time on Recombinant vaccines, DNA vaccines, Bioinformatics, microarray and other eras of molecular Biotechnology.
Abstract:
Background and Objective: Biological weapons like other weapons of mass destruction, including nuclear and radiological weapons are very dangerous in recent years due to characteristics such as the ability to create extensive injury , having incubation period , creating long illness , the ability to spread and epidemic and most importantly non-specific symptoms and difficulty in detection of bioterrorism attacks are increasingly used by some countries . One of the most important steps to deal with the Bioterrorism threat is microbiological detection of biological agents that can be done in the Microbiology laboratory.
Methods: This study aimed to review the role and actions of microbiology laboratories and specialists needed in passive defense against biological threats. In this study databases like CDC, Medline, Google scholar, PubMed and the World Health Organization (WHO) and other national and international sources have been used.
Results: The basic principle of control bioterrorism attacks is based on the ability to rapidly deliver health services . Microbiology laboratories play a critical role in the rapid and accurate detection of biological agents due to the lack of features such as odor, color and other physical characteristics, diagnosis is difficult and sometimes impossible.Therefore Microbiology Laboratories should be equipped with advanced detection and diagnosis methods along with rapid development of Novel biological Agents and Personnel should be trained with current detection methods and protocols and further with biosafety and biosecurity guidelines for working with bio agents.
Conclusion: With rapid Development in detection systems and methods specially molecular detection protocols and instruments for Biological Agents it will be nesecary for nationas Microbilogy laboratoryies and personel to be trained and equiped and redy for detection of any possible biological incidents.
- Track 1:Viral Infectious Diseases
Track 2:Bacterial Infectious Diseases
Track 3:New Antiviral, Antibacterial and Antifungal Agents
Track 4:Bacterial Susceptibility & Resistance
Track 5:Nosocomial Infections
Track 6:Vaccines
Track 7:Respiratory Diseases
Track 8:Protozoal Diseases
Track 9:Infectious Disease Epidemiology
Track 10:Emerging Infectious Diseases
Track 11:Infectious Diseases in Asia
Location: Paris, France
Session Introduction
Catherine Mullié
University of Lille
Title: Comparison of efflux pumps expression in ciprofloxacin-resistant Pseudomonas aeruginosa clinical and environmental strains from Algeria and France.

Biography:
Catherine Mullié obtained a PhD in Microbiology and a PharmD at the University of Lille, France, in 1999. After a post-doc year at the Faculté de Medicine in Amiens (Laboratoire d’Immunologie, INSERM-EMI 0351), she was appointed as assistant professor at the Faculté de Pharmacie in Amiens in 2000 and joined the LG-2A (Laboratoire de Glycochimie des Antimicrobiens et des Agroressources, UMR 7378 CNRS) in 2008. She has been a member of the French Society for Microbiology since 2000. Her research is focused on the development of new antimicrobial and antimalarial drugs, with a special interest in efflux-mediated antibiotic resistance in Pseudomonas aeruginosa and Acinetobacter baumannii. She currently heads the French part of a bilateral project funded by France and Algeria (Partenariat Hubert Curien Tassili) on this topic.
Abstract:
Statement of the Problem: Pseudomonas aeruginosa is a Gram-negative ubiquitous microorganism found in various environmental niches as well as in human infections. It is innately resistant to a large number of commercially available antibiotics and has acquired a wide array of resistance mechanisms, tremendously complicating the clinical handling of P. aeruginosa infections. Antibiotic resistance can be mediated by several molecular mechanisms, one of them being the efflux of antibiotics from the bacterium through efflux pumps. In P. aeruginosa, antibiotic efflux is mainly mediated by pumps belonging to the Resistance-Nodulation-Division family: MexAB-OprM, MexCD-OprJ, MexEF-OprN and MexXY-OprM. This work aimed to compare their expression in environmental and clinical strains of P. aeruginosa from Algeria and France either resistant or susceptible to fluoroquinolones to evaluate whether expression patterns would vary according to the sample origin and/or country.
Material & Methods: Clinical strains were collected from Amiens & Lille hospitals for France and Saida hospital for Algeria. Environmental strains were mostly isolated from water samples. Susceptibility to ciprofloxacin was evaluated by E-test and the broth microdilution method with and without an efflux inhibitor. Efflux pumps expression was then measured through a qRT-PCR experiment, using mexB, mexD, mexF and mexY as target genes.
Findings: 149 clinical and 30 environmental P. aeruginosa strains were included. According to EUCAST breakpoints, 29.8% and 11.1% of French and Algerian clinical strains were resistant to ciprofloxacin, respectively. None of the environmental strains were resistant to ciprofloxacin. Analysis of qRT-PCR data showed that mexY expression was significantly increased in a majority of ciprofloxacin-resistant clinical strains while mexA was decreased.
Conclusion & Significance: This study showed that ciprofloxacin-resistant strains were more common in clinical P. aeruginosa isolates than in environmental one. The design of efflux inhibitors targeting MexXY-OprM efflux pump could therefore be of use to restore the activity of known antibiotics.
Philip Norrie
Universities of New South Wales, Australia
Title: A HISTORY OF INFECTIOUS DISEASE IN ANCIENT TIMES – MORE LETHAL THAN WAR - AN ALTERNATIVE MEDICAL HISTORY PERSPECTIVE OF ANCIENT HISTORY

Biography:
Dr. Philip NORRIE MBBS,MA,MSc,MSocSc[Hons],PhD,MD,MPhil[cand] is a family physician from Sydney, Australia whose main interest is medical history. This medical history interest is in two parts. Firstly in the history of wine as a medicine for the past 5,000 years which was the topic of his PhD. After this Dr. Norrie developed the world’s first fully Resveratrol Enhanced Wine [REW]. The second interest is the role of infectious disease in the demise of ancient civilizations, which was the basis of his MD thesis and his current M.Phil thesis. Dr. Norrie is a Conjoint Senior Lecturer at the Faculty of Medicine at the Universities of New South Wales and Newcastle in Australia; as well as being an Affiliate in Medical History at the University of Montana,USA, an Adjunct in the National Institute of Complementary Medicine at the Western Sydney University [relating to REW]and the Vice Chairman of the Medical Advisory Committee at the Northern Cancer Institute in Sydney.
Abstract:
“Historians find war exciting and pestilence dull; they exaggerate the effects of the former and play down the latter.” (Grove and Rackham 2001)
When one thinks of ancient history one thinks of ancient historians and archaeologists; one does not think of medical historians. But one should because most major changes in the ancient world were precipitated by an infectious disease epidemic of some kind. It is very naïve of ancient historians not to factor in the possibility that an infectious disease epidemic ended the civilization they are studying because it would have been a daily struggle NOT to die from an infectious disease in the ancient world. Hence the possibility of an infectious disease epidemic is the FIRST thing ancient historians should eliminate during their research.
This lecture will discuss the possibility of such an occurrence happening firstly in Sumer c.2000 BCE, the site of the world’s first cities (1), followed by the Indus Valley Civilization c.1900 - 1350 BCE (2), Pharaonic Egypt during the 18th Dynasty c.1350 BCE (3) (4), Haft Tappeh in Elam c.1350 BCE (5),then the end of the Hittite Empire c.1200 BCE (6) and finally the end of the Bronze Age in the Near East c.1200 BCE (7).
This hypothesis challenges the current ancient history theories for the end of these civilizations and will upset ancient historians trained in the arts and not trained in using the medical model; which unfortunately is the vast majority. Infectious diseases such as influenza, measles, polio, tuberculosis, dysentery, malaria, typhoid, leprosy and finally the “big two” infectious disease epidemics namely smallpox and plague; decimated the ancient world.
Siyu Zhu
Tsinghua University, China
Title: Structure-based discovery of potential small-molecule inhibitors targeting Zika virus NS3 helicase

Biography:
Abstract:
Zika virus (ZIKV) is a mosquito borne pathogen that has been rapidly a rapidly expanding epidemic across Central and South America since 2015. It belongs to flavivirus family and is closely related to Dengue virus and West Nile virus. ZIKV was first isolated in 1947 from a rhesus monkey around the Zika forest of Uganda. ZIKV has been realized as a major health risk, making it a compelling target for viral therapeutics. Its infection causes not only mild symptoms such as fever, headache, arthralgia and conjunctivitis, but frightening neural diseases including Guillain–Barré syndrome, congenital microcephaly, as well as macular atrophy. There’s an urgent need to discover and develop direct-acting antiviral agents (DAAs) in view of the current lack of effective medicine for ZIKV. Nonstructural protein 3 (NS3) helicase of ZIKV is considered to be essential for viral replication and have become an attractive target for the development of DAAs. Recent years, in silico virtual screening has been generally accepted as a rapid, efficient, economical approach with low time and labor cost for screening a large set of compounds. Here, an in-silico screening analysis of NCI diversity dataset with ZIKV NS3 protein targets has been carried out using a structure-based molecular docking approach. A total of 1974 compounds with structural simplicity and diversity have been docked. Top-ranked 5% of compounds with drug-like properties were selected for antiviral evaluation by cell-based ZIKV infection assays. Three hits were identified to specifically inhibit the viral infection with EC50 values at a micro-molar level. Different series of potential derivatives with expected better antiviral activities were presented based on similarity search and target-ligand binding modes. Overall, the discovery of these NS3-targeting compounds may serve as novel leads for further optimization and development of clinical ZIKV inhibitors.
Maha Gaafar
Alexandria University, Egypt
Title: Chitosan and silver nanoparticles: promising antitoxoplasma agents

Biography:
Maha Gaafar has her expertise in diagnosis of different parasitic infections in various samples; blood, stool, urine and aspirates using novel and rapid techniques as enzymatic assays and real-time PCR. Her trials in treatment of the most common infectious diseases based on the use of new and safe lines of treatment as herbal treatment as well as the use of nanoparticles either natural or metal as anti-parasitic agents.
Abstract:
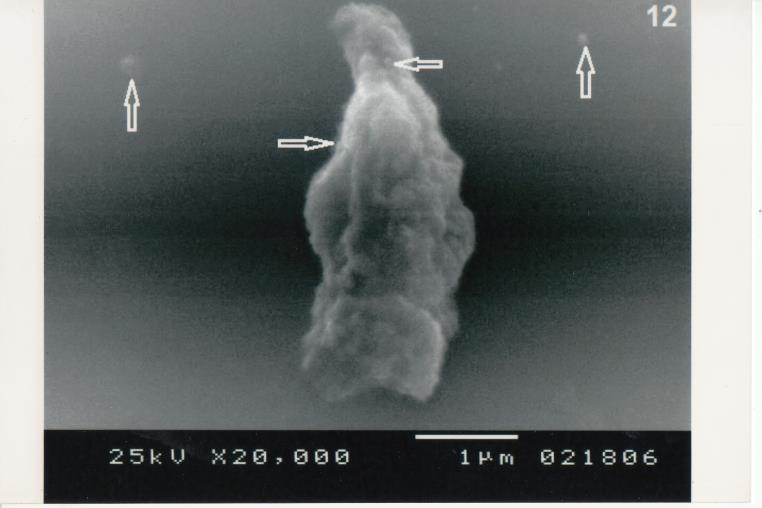
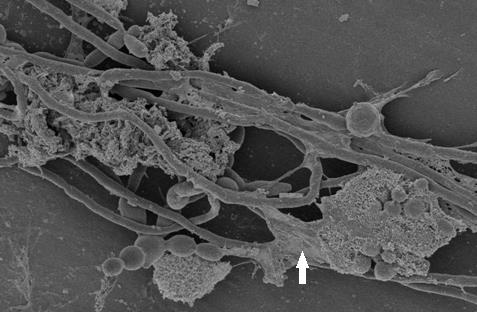
Toxoplasmosis is a worldwide infection caused by obligate intracellular protozoan parasite which is Toxoplasma gondii. Chitosan and silver nanoparticles were synthesized to be evaluated singly or combined for their antitoxoplasma effects as prophylaxis and as treatment in the experimental animals. Results were assessed through studying the parasite density, studying the ultrastructural parasite changes and estimation of serum gamma interferon. Weight of tissue silver was assessed in different organs. Results showed that silver nanoparticles used singly or combined with chitosan have promising antitoxoplasma potentials. The animals that received these compounds showed statistically significant decrease in the mean number of the parasite count in the liver and the spleen, when compared to the corresponding control group. Light microscopic examination of the peritoneal exudates of animals receiving these compounds showed stoppage of movement and deformity in shape of the tachyzoites, whereas, by Scanning Electron microscope, the organisms were mutilated. Moreover, gamma interferon was increased in the serum of animals receiving these compounds. All values of silver detected in different tissues were within the safe range. Thus, these nanoparticles proved their effectiveness against the experimental Toxoplasma infection.
Ali Harb
Murdoch University, Australia
Title: Prevalence, Antimicrobial Resistance and Risk Factors of Salmonella Diarrheal Infection among Children in Thi-Qar Province, Iraq

Biography:
Ali has worked as a head of the investigation team for communicable disease in Thi-Qar Public Health Division, Ministry of Health, Iraq. Ali was graduated with a Bachelor in Veterinary Medicine in 2003 and an MSc. in Zoonotic disease in 2010 from Baghdad University, Iraq. Currently, Ali is a PhD student in epidemiology and infectious diseases. His PhD research is about investigating the transmission routes of community-acquired Salmonella infection in Iraq. Ali collected human and foods samples from Iraq. Ribotypes of interest will undergo whole-genome sequencing (WGS) to determine the genotypic diversity and correlation between Salmonella isolates from human diarrhea and foods. Ali also conducted two surveys to determine the risk factors of diarrhea illness and Salmonella infection among children under five years. His research will provide a better understanding of the mode of transmission of Salmonella spp from food sources to cause infections in humans.
Abstract:
Statement of the Problem: Salmonellosis is one of the most common bacterial diarrheal illnesses among children and poses a significant public health burden worldwide; despite this fact, data on non-typhoidal Salmonella spp in Iraq are limited. The current study therefore aimed to determine the prevalence, clinical presentation, serotype and antimicrobial resistance profiles, and risk factors associated with Salmonella infection in children in Thi-Qar province, south-eastern Iraq. Methodology & Theoretical Orientation: This hospital-based cross-sectional study among children aged less than 5 years presenting with diarrhoea at paediatrics hospitals. Stool samples were identified using conventional and molecular methods. Antimicrobial susceptibility testing was performed using disk diffusion method. The associations between stool-culture positivity for Salmonella spp. and risk factors were assessed by Odds Ratio (OR), and 95% Confidence Intervals (CIs) was considered significant at P-value ≤ 0.05. Findings: From 320 diarrhea cases enrolled between March and August 2016, 33 (10.3%) diarrhea cases were stool culture-positive for non-typhoidal Salmonella. Resistance was most commonly detected against tetracycline (78.8%), azithromycin (66.7%), and ciprofloxacin (60.6%). The multivariable logistic regression analysis indicated that higher odd of Salmonella infection in children from household associated with untreated water (pipe water) (OR= 4.7 (95% CI: 1.6, 13.9), exposure to domestic animals (OR= 10.5; 95% CI: 3.8, 28.4) and low education level of the caregiver (OR= 3.9; 95% CI: 1.0, 6.4). Lower odd of Salmonella infection were associated with children exclusively breastfed (OR= 0.4; 95% CI: 0.1, 0.9) and caregiver those always washing hands after cleaning child defecation (95% CI: 0.1, 0.7). Conclusion & Significance: Our findings indicate that Salmonella is an important cause of children diarrhea in this setting. This work provides local, specific epidemiological data which are crucial to understand and combat pediatric diarrhea in Iraq.
Monica Pia P. Reyes
St. Luke’s Medical Center Global City, Philippines
Title: Cytomegalovirus-Varicella Zoster Meningoencephalitis and Ischemic Stroke in an HIV-AIDS patient: a Case Report

Biography:
Monica Pia P. Reyes, MD is a licensed physician since 2013. She is currently a 3rd year Internal Medicine Resident at St. Luke’s Medical Center- Global City, Philippines and is planning to subspecialize in Infectious Diseases. She is currently the Resident Head of the Committee on Internal Academics and Research. Her interest in research got her to present oral cases and posters in some specialty conventions in Manila.
Abstract:
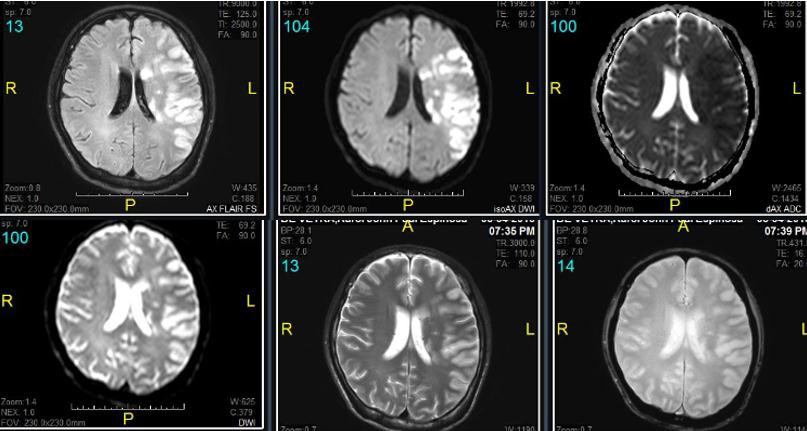
Along with the increasing number of newly diagnosed Human Immunodeficiency Virus (HIV) patients per day in the Philippines (26 new cases/day)1 is an increasing number of HIV patients diagnosed with Central Nervous System Infection (CNSI) and Stroke. A study shows that the risk of ischemic stroke was higher among those with HIV infection compared with uninfected people (hazard ratio 1.17)2. Mechanisms of ischemic stroke include HIV-associated vasculopathy, opportunistic infections or neoplasia, cardioembolism and coagulopathy3. This case report aims to present a CNS co- infection of the three most documented viruses that causes stroke: Cytomegalovirus (CMV), Varicella Zoster Virus (VZV) and HIV. The inflammatory cascade in these infections promotes atherosclerosis, plaque rupture, and thrombosis, leading to ischaemic stroke4. A 35-year-old male with HIV who is non- compliant with anti-retroviral therapy and who had recent untreated Shingles was brought in with decreased sensorium, signs of meningeal irritation and right-sided neurologic deficit. Computed Tomography scan revealed cute to Subacute Infarct, Left Middle Cerebral Artery Territory (Figure 1). He was admitted and started empirically on Vancomycin, Ampicillin, Cefepime and Ganciclovir for Central Nervous System Infection. HIV work-up revealed a CD4 of 11 cells/mm3 and HIV-1 RNA of 1,124,215 copies/mL. CMV IgG is positive at 65 U/mL. Lumbar tap done had an elevated opening pressure with elevated cerebrospinal fluid (CSF) protein, low- normal CSF glucose, and pleiocytosis with lymphocytic predominance. Viral panel showed CMV viral load of 634,000 copies/mL and VZV IgG 44.4mIU/L clinching the diagnosis of concomitant CMV-VZV meningoencephalitis in this HIV patient. Magnetic Resonance Imaging and Angiogram is compatible with viral vasculopathy (Figure 2). The pathogenic mechanisms of VZV reactivation in the CNS include neuronal and glial direct infection and immune-mediated lesions including vasculitis and demyelinization5 while CMV infection of vascular smooth muscle cells induces production of powerful pro-inflammatory cytokines which accelerate atherosclerosis development6. This might be the first reported case of co-infection of the CMV- VZV-HIV meningoencephalitis and Ischemic Stroke.

Omar Nafi
Mutah university, Jordhan
Title: Mediterranean Spotted Fever in Children of the Karak Province in South Jordan

Biography:
Dr.Omar Ali Dahoud Nafi Pediatric neurologist Associated professor of pediatrics Place and D.O.B.: Naur ,Jordan 1953 Male , Jordanian , Married Mutah University- College of medicine - Pediatrics department
MBBS in medicine 1980 from Cordoba University – Spain 2- -Jordainan board in pediatric 1986 3- training in pediatric neurology in Dublin – Ireland 1997 4--(MRCP) Membership of royal collage of physician of Ireland in pediatric 2000
Abstract:
Introduction: The aim of this study was to describe the epidemiological patterns of Mediterranean spotted fever (MSF) as well as its treatment and outcomes in children in south Jordan.
Methodology: We conducted a retrospective observational study from June 2013 to December 2015. Data regarding demographics, clinical presentation, laboratory findings, treatment, and outcomes were collected.
Results: Thirty-five male and 20 female patients (mean age: 6 years ± 3.6) were included. The incidence of MSF was 7.9 cases per 100,000 inhabitants/year; MSF affected 89% of individuals in the summer, 74.5% of those living in a rural area with tent housing, and 100% of those who had contact with animals. All cases presented with fever, and 94.5% had a skin rash. Serological tests were positive in 87.2% of cases, and Rickettsia conorii (the Moroccan strain) was present in all positive cases. All cases had thrombocytopenia, but none had leukocytosis. Hyponatremia was present in 71% of cases, and 49%, 61.8%, and 72.7% had increased urea, alanine transaminase, and aspartate aminotransferase levels, respectively. Doxycycline was administered to all patients, with a cure rate of 96.4% and mortality rate of 3.6%.
Conclusions: MSF caused by R. conorii (the Moroccan strain) is prevalent in Jordan, and contact with animals is a common route of transmission. The patients’ responses to doxycycline were excellent. A high index of suspicion, an early diagnosis, and specific

Biography:
A results oriented health management professional with years of experience in providing technical and managerial assistance in the areas of public health training, capacity building, knowledge management/ research and project management. I have demonstrated expertise in organizational/technical assessments and building capacity as the practice head of a public health consulting firm in Kolkata. At present, associated as Capacity Development Advisor of Tuberculosis Health Action Learning Initiative (THALI) project being implemented by John Snow India Private Limited, indian subsidiary of John Snow Inc. US
Abstract:
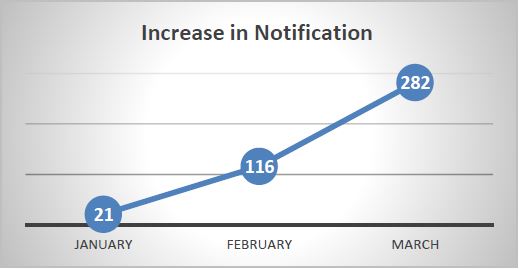
Statement of Problem: India’s private sector is treating an enormous number of patients for tuberculosis, appreciably higher than has been previously recognized. Prompt notification to the public health system is an important component of the TB surveillance and controlling TB. Poor notification of TB cases from private sector, in Kolkata, second largest city of India is a concern. This study aimed to determine the yield of providing ICT support to private doctors to notify TB cases and assess the increase in TB case notification in Kolkata. Methodology: An observational study was done over three months involving 174 private doctors treating TB, who were earlier not notifying TB cases. They were provided technical inputs on how to notify TB cases through trainings and logistics support was extended through ICT based call center dependent platform to notify TB cases. Findings: Of 174, 63% doctors started to notify TB cases regularly and notified 419 cases of TB. The notification showed an increasing trend with increase during the last month which coincided with increase in technical inputs through trainings and one-to-one interactions. Conclusion and Significance: The 419 cases notified in three months, is close to the annual notification of 679 TB cases, as per 2016 TB report, from private sector in Kolkata. The real-time ICT solution which takes away the demand on time of the private providers to notify proved to be a success to boost private sector TB notification in Kolkata. Further observance may be required over a longer period of time, with a larger group of private providers to evaluate the effectiveness of the intervention.
Tereza Jancuskova
Charles University, czech republic
Title: Molecular microbiology as a modern platform for rapid, specific, sensitive and unlimited detection of pathogenic microorganisms

Biography:
Tereza Jancuskova graduated from the Faculty of Science, Charles University in Prague, Czech Republic in 2008. She continued her PhD. studies at the Third Medical Faculty, Charles University in Prague, specializing in genetics, molecular biology and virology. She received her PhD. degree in 2015. Tereza Jancuskova has extensive expertise in molecular hemato-oncology and molecular genetics, both in human and veterinary medicine.
Abstract:
Molecular microbiology is a novel concept that opens up fascinating possibilities in the pathogen detection. Many microorganisms are fastidious or uncultivatable; their cultivation time is unacceptably long; are of high epidemiological importance; or require sophisticated cultivation conditions. Molecular techniques allow for quantitative detection of microorganisms based solely on the presence of their unique DNA or RNA sequences. Molecular microbiology enables to identify causative infectious agents even in those situations when standard cultivation-based microbiology fails.
Since 2006, we have developed over 500 single and multiplex quantitative Real-Time PCR assays to detect pathogenic and opportunistic infectious agents relevant for both human and veterinary clinical settings. We have implemented pandetection approach to detect bacteria and fungi based on Sanger sequencing. For the most challenging biological samples (gut microbiome) we have also developed a pandetection strategy based on Next Generation Sequencing (NGS). Using this combined approach, we are able to identify microbial agents with the widest detection range possible (pandetection), quantify the load of individual microorganisms in the sample and provide the clinician with the result within hours (Real-Time PCR), or 2-3 days maximum (Sanger sequencing or NGS).
Over the past 10 years we have diagnosed more than 30,000 biological samples, originating from both human and veterinary patients. They covered hyperacute clinical settings (sepsis), chronic and underdiagnosed diseases, and emerging zoonoses (our finding of a novel zoonotic agent Candidatus Neoehrlichia Mikurensis, transmissible by a tick bite, with unexpected Central and Western European geographic occurrence).
Jenny Mae A. Quinivista-Yoon
St. Luke’s Medical Center, Phillipines
Title: Toxic Shock Syndrome due to Streptococcus pyogenes in an 80-year old post-Knee Arthroplasty Patient: A Case Report.

Biography:
Jenny Mae A. Quinivista-Yoon is currently a second year Internal Medicine Resident at ST. Luke’s Medical Center-Global City in the Philippines who aspires to become a relevant Infectious Disease specialist in the future. Her current interests in the Infectious Disease field include nosocomial infections and their prevention, as well as community-onset disease outbreaks
Abstract:
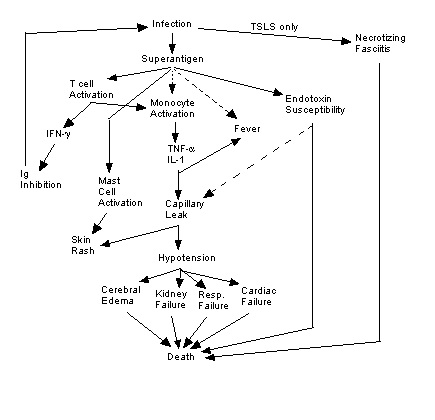
Prosthetic joint infection (PJI is one of the leading causes of arthroplasty failure. A high incidence of PJI follows Staphylococcus aureus and coagulase-negative staphylococci. On the other hand, Streptococcus pyogenes PJI is extremely rare, with only a very few case reports in the literature. Toxic Shock Syndrome resulting from Streptococcus pyogenes infection, however, has a reported mortality rate as high as 30 to 70 percent, hence early recognition of this potentially fatal infection is crucial to the successful management of patients. In this article, we report a case of an eighty-year old male who developed streptococcal toxic shock syndrome in association with a severe group-A streptococcal infection of the knee after a total knee arthroplasty done two years prior.

Biography:
Fentabil Getnet Yimer has expertise in medical microbiology and public health researches focusing on communicable diseases with special emphasis on Tuberculosis. My PhD research project is on Delay in Diagnosis of pulmonary tuberculosis and its effect on household contact transmission. This study has aimed to investigate the extent, determinants of delayed care and the extent it impacts the household members of tuberculosis patients in a pastoralist setting.
Abstract:
Assessment of time delays in diagnosis of tuberculosis is essential to evaluate effectiveness of control programs, and identify programmatic impediments. Thus, we have reviewed recent studies to summarize patient, health system and total delays in diagnosis of pulmonary tuberculosis and associated factors with it in low- and middle- income countries.
The review was done following standard procedures of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and checklist. Web-based databases were searched to retrieve relevant studies from 2007 to 2015 including Springer link, Pubmed, Hinari and Google scholar. Searching terms were pulmonary tuberculosis, diagnostic delay, patient delay, health system delay, provider delay, doctor delay, health care seeking and health care seeking behavior. Retrieved studies were summarized by systematic review and meta-analysis using comprehensive meta-analysis software.
Forty studies involving 18,975 patients qualified for systematic review and 14 of them for meta-analysis. The reported median total delay ranges from 30 to 366.5 days; with a relatively more for patient delay (4 to 199 days) compared to health system delay (2 to 128.5 days).The key determinants of patient delay were poor literacy, long distance to the nearest health facilities, evil/bad luck perception as cause, poor knowledge, first care seeking from informal providers, self-medication, pulmonary co-morbidity and mild severity of illness among others. Likewise, good functional status, unusual symptoms, first care seeking at private and low level facilities, normal chest X-ray and smear negative results were key determinants of health system delay. The meta-analysis showed 42% of pulmonary tuberculosis patients delayed seeking care by a month or more; uneducated patients [pooled OR=1.5, 95%CI=1.1-1.9] and those who sought initial care from informal providers [pooled OR=3, 95%CI=2.3-3.9] had higher odds of patient delay.
Fernanda de Freitas Anibal
University of São Paulo, Washington USA
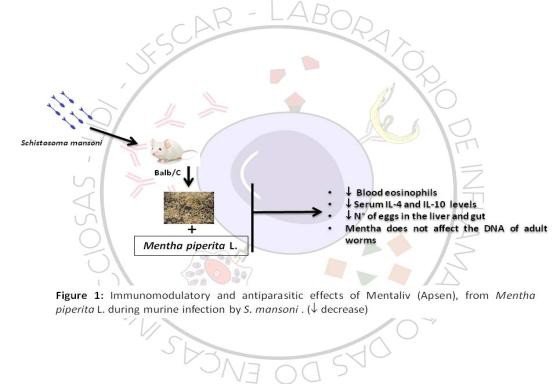
Title: Phytotherapy from Mentha piperita L. modulates infection during experimental schistosomiasis

Biography:
Fernanda de Freitas Anibal had her PhD from University of São Paulo, Brazil in Basic and Applied Immunology. She is a Principal Investigator at Laboratory of Inflammation and Infectious Diseases (Federal University of São Carlos) seeks new tools for the treatment, prevention and diagnostics for infectious diseases. Currently, they are working with two plants and six enzymes and their effects against schistosomiasis mansoni, leishmaniasis and toxocariasis, about the treatment of the infectious diseases. Their group studies effects of plants (extracts) and their isolated fractions in order to evaluate the anti-parasitic and anti- inflammatory effects and for infectious disease prevention, moreover have been working on the evaluation of the proteins of the parasite that has been potential to induce immune responses that decrease the parasite burden.
Abstract:
Schistosomiasis is a chronic parasitic disease promoted by the parasite of the genus Schistosoma, and Praziquantel (PZQ) is the only drug recommended by the World Health Organization, but there are reports of resistance, suggesting the importance of studying new compounds to treat this disease. In this work we investigate the immunomodulatory and antiparasitic effects of Mentaliv (Apsen), from Mentha piperita L. during murine infection by S. mansoni (Sm). Experimental groups: Balb/c females, (I) C, uninfected, (II) SM, infected without treatment, (III) Mentha 15 (50mg/kg) infected with Sm (80 cercariae/animal) (IV) Mentha 60 (50 mg/kg), infected and treated daily for 60 days and (V) PZQ, infected and treated with single dose (400mg/kg) at the 43rd day after infection. The cell profile in the blood and serum IL-4 and IL-10 cytokines were analyzed. And the antiparasitic effect on egg count in the liver, intestine and granulomas, and comet assay for DNA modifications in worms recovered after treatments. Mentaliv phytotherapy has immunomodulatory and antiparasitic effects during murine infection of experimental schistosomiasis, by reducing serum levels of IL-4 and IL-10, and indirectly modulating negatively the blood eosinophils in the Mentha 60 group. In addition, there is an antiparasitic effect in these animals of the Mentha 60 group where there is a reduction in the number of eggs in the liver, intestine and in the hepatic granulomas. However, the absence of the genotoxic effect on Sm, suggests that other structures of the parasite other than DNA are being altered and thus contributing to the reduction of parasitic load. Thus, it is suggested that menthol and menton may be the main components of Mentha piperita L. with antiparasitic effect in this model.
Arnaud Avril
Institut de Recherche Biomédicale des Armées (IRBA), France
Title: Development of five hyper-humanized antibodies neutralizing the Botulinum neurotoxins A, B and E: the European AntiBotABE project.

Biography:
Dr. Arnaud AVRIL works for the French Armed Forces Biomedical Research Institute (IRBA), based in Paris area. He has a master degree in genetic and immunology from Lyon University (France) and a PhD in biotechnology applied to antibodies from the Grenoble-Alpes University (France). He is the head of a team specialized in the research, development and engineering of recombinant antibodies against rare diseases for biodefense. He developed germline-humanized recombinant antibodies starting from non-human primates immunized with non-toxic antigens. He contributed to the development of several antibodies neutralizing botulinum neurotoxins, anthrax, ricin and orthopoxviruses. He also contributed to the development immuno-diagnostic assays for the rapid, convenient and cheap detection of biological agents, for armed forces, medical staff and first responders. He is involved as an expert on the clinical development of a recombinant antibody for anthrax therapy.
Abstract:
Botulism is a naturally occurring disease, mainly caused by the ingestion of food contaminated by one of the 7 serotypes (A to G) of botulinum neurotoxins (BoNTs). BoNT/A is the most lethal biological substance currently known, with a human 50 % lethal dose estimated at 1 ng.kg-1, and they are classified among the 6 major biological warfare agents. AntiBotABE (www.antibotabe.com), a European Framework 7 funded project aimed to develop 6 humanized IgGs, neutralizing BoNT serotypes A, B and E by targeting their heavy (HC) and light chains (LC). Six macaques were immunized with the recombinant LC or HC of BoNT/A, B or E, and their corresponding immune libraries were generated and screened by phage-display. After each panning, the most reactive scFv were isolated and their affinity measured. Inhibition or neutralization capacities were determined in vitro (SNAP25 or VAMP2 endopeptidasic assay) or ex vivo (mouse phrenic nerve-diaphragm assay). Neutralizing scFvs were identified for 5 of the 6 antigens. For each of the 5 libraries, the most efficient scFv was germline-humanized and expressed as full-length IgG. In the mouse bioassays, 3/5 IgGs alone and all IgGs in pairs, protected mice from paralysis or death after a challenge with the respective BoNT serotype. 1–5Antibodies isolated during this project are potential lead candidates for further clinical development and we are looking for clinical development opportunity.
Nid’a H. Alshraiedeh
Jordan University of science and technology, Jordan.
Title: In vitro evaluation of the impact of APNTP pre-exposure on antibiotics susceptibility of Pseudomonas aeruginosa biofilms.

Biography:
Nid’a Alshraiedeh has done her PhD in pharmaceutical microbiology at Queen’s university Belfast. She has an expertise in APNTP and antimicrobial resistance. Currently Nid’a is an assistant dean at JUST nanotechnology institute and assistant professor at school of pharmacy, JUST. She has 2 projects running; one about Cystic fibrosis pathogens and antimicrobial resistance among the isolated pathogens. 2nd project is about using nonpathogenic microorganisms as a nanorobots for drug delivery. her PhD was mainly on use of APNTP to control pathogens associated with hospital acquired infections and after finding promising results, she is still interested in research in this field and planning to do further research.
Abstract:
Statement of the Problem: Biofilms are the predominant mode of bacterial growth in the environment. They are implicated in approximately 80 % of chronic human infections (Kalmokoff 2006; Francolini 2010). its formation is associated with high tolerance to conventional biocides and antimicrobial agents (Nandakumar 2004; Kamgang 2007). Tolerance could be attributed to impaired diffusion, neutralising mechanisms, presence of persister cells, acquiring resistant genes and other factors that could work synergistically to develop resistance (Costerton 1999; Parsek 2004).
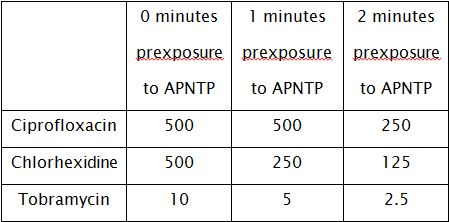
Findings: A preliminary study was conducted to assess the potential use of in-house designed kilohertz (kHz)-driven atmospheric pressure non-thermal plasma (APNTP) as adjuvant therapy with other available antimicrobial agents that are commonly used for the control of Pseudomonas aeruginosa infections, and whose activity are known to be attenuated in the presence of biofilm matrix components. Synergy between APNTP pre-exposure and the antibiofilm activity of three antimicrobial agents (ciprofloxacin, tobramycin and chlorhexidine) was demonstrated. Pre-exposure of a 48 hour biofilm to APNTP increased the sensitivity of Pseudomonas aeruginosa biofilm to the tested antimicrobial agents. Further studies have been conducted to understand the factors that increase the sensitivity of APNTP treated biofilm to tobramycin. Effect of initial bacterial titers on sensitivity to tobramycin was negligible. The protective effect of EPS was also studied and found that Pre-exposure of exogenous DNA and alginate to APNTP did not appear to restore the sensitivity of Pseudomonas aeruginosa to antimicrobial agents.
Conclusion & Significance: This study showed a promising results for possibility of use sub-optimal exposures of APNTP as adjuvant topical therapy with conventional antimicrobials agents. Further studies are required to explain the mechanism underlying this synergy in order to provide important information for the design and optimization of non-thermal plasma sources for infection control.
Ahmad M. Domado
Southern Philippines Medical Center, Philippines
Title: Streptococcus suis: Bacteremia presenting with Fever, Rashes, Arthritis and Neurologic Deficits.

Biography:
Abstract:
Streptococcus suis (S. suis) is a gram positive cocci acquired through exposure to infected swine. The most common clinical manifestation is meningitis often accompanied by bacteremia. S. suis is an emerging pathogen with significant complications, but remains to be underreported. Only 1,584 cases of S. suis infection have been reported worldwide with most of the cases concentrated in Southeast Asia where swine quantity is high. Despite a booming hog industry in the Philippines and increasing prevalence in its neighboring countries, S. suis infection remain unreported in our country due to either lack of available diagnostics or misdiagnoses. We report a case of a 52-year-old male who came in due to fever, generalized violaceous purpuric rash, headache, and nuchal rigidity. Patient was diagnosed with meningitis clinically. Patient consumed a diseased swine 5 days prior to admission. Blood culture was positive for Streptococcus suis II and clinical improvement was achieved with antibiotic treatment. Our patient is the second Filipino and the first documented case to be diagnosed in the Philippines. Patient is also the first documented case of a Filipino with Streptococcus bacteremia presenting with meningitis, hearing loss, skin lesions and arthritis. In S. suis infection, antibiotic treatment should be started without delay because a high mortality rate of up to 68% is observed in patients with septicemia and septic shock. With increased awareness and available diagnostics, a future outbreak, can be prevented.
Gaurav Gupta
All Institute of Medical Sciences, New Delhi
Title: Adverse events in patients with Multidrug-Resistant Tuberculosis: Results of a prospective cohort study at tertiary care level

Biography:
Abstract:
BACKGROUND: Drug resistance Tuberculosis (DR-TB) is a public health crisis and its diagnosis and management is challenging task. One of the major obstacles in achieving successful treatment outcomes in DR-TB are adverse events affecting the adherence to the second line drugs (SLD).
OBJECTIVE: To evaluate the frequency of adverse events due to the second line drugs in Multidrug-Resistant Tuberculosis (MDR-TB) patients.
METHODS: A prospective cohort study was conducted at DOTS Plus site at AIIMS, New Delhi .The cohort of 81 MDR-TB were recruited between June 2014 to June 2016 and were provided with standardized RNCTP regimen. Patients were followed up and adverse events were primarily recognized with clinical evidence and/or laboratory investigations. Data was collected in pre-designed proforma. The data was analyzed by stata 14 and presented in mean (standard deviation)/median (min to max) and frequency (%) with confidence interval (95%).
RESULTS: 91 adverse events were reported in 52(64.1%) patients. Only 1.2 %( 1/81) of the patient stopped treatment, but 9.8% (8/81) required removal of the suspected drug(s) from the regimen due to adverse events. The grouped adverse events were most commonly gastrointestinal (70.6%), arthralgia (10.9%), ototoxicity (6.4%), psychiatric (5.5%), and hypothyroidism (2.1%).Eight (9.8%) patients had major adverse events requiring discontinuation or substitution of drugs that included psychiatric disturbances in 5(6.1%) followed by hearing loss and tinnitus in 3(3.7%).
CONCLUSIONS: In India Programmatic management of drug resistance tuberculosis (PMDT) guidelines provides excellent guidance for diagnosis and treatment of DR-TB. Adverse events can be catered if addressed at the time by the health care system and adherence can be assured for successful treatment outcomes.
Ram Prakash Thirugnanasambandam
Sri Ramachandra Medical University, India
Title: ADENOVIRUS-ROUGH N TOUGH: SUCCESSFUL TREATMENT OF DISSEMINATED ADENOVIRUS INFECTION IN TWO SOLID ORGAN TRANSPLANT RECIPIENTS

Biography:
Abstract:
Adenovirus is a DNA virus that causes infections of the respiratory tract, gastrointestinal tract, conjunctiva and rarely urinary or neurological systems. Disease caused by adenovirus is usually self-limiting but it can cause disseminated infection with high morbidity and mortality. We present two cases of transplant recipients who developed disseminated adenovirus infection and were successfully treated on a compassionate basis with the investigational drug Brincidofovir.
The first patient is a 47 year old female with kidney/pancreas transplant done 6 months prior to presentation who was admitted with hematuria for 9 days, fever and acute kidney injury. A cystoscopy was done which revealed erythema in the bladder and transplant ureter. Biopsy of transplanted kidney was PCR positive for adenovirus and had changes consistent with adenovirus tubulo-interstitial nephritis. Due to pancytopenia, she underwent a bone marrow biopsy which was PCR positive for adenovirus. She was started on cidofovir but quickly developed worsening renal failure, hence she was switched to brincidofovir. Within 3 weeks of starting treatment, her symptoms resolved and adenovirus PCR was negative in urine. Unfortunately her renal function did not improve and she remains on hemodialysis.
The second patient is a 46 year old African American female who underwent Deceased Donor Kidney Transplant (DDKT) 4 months prior to presentation. She presented with fever for 2 days, abdominal pain and non-bloody watery diarrhea. Temperature was 103 F and she had pancytopenia. On labs, pertinent negatives included urine culture, blood culture, serum PCR for CMV and EBV and stool studies. Adenovirus was detectable by PCR in urine and was positive in blood with 11,571 copies detected. Due to pancytopenia, she had a bone marrow biopsy which was PCR positive for adenovirus. She was diagnosed with disseminated adenovirus infection and was initiated on brincidofovir with improvement in fever and diarrhea. Due to our experience with the first patient we were hesitant to initiate cidofovir. At one month follow up, blood cell counts had improved and adenovirus PCR in blood and urine were both undetectable.
Brincidofovir is an investigational drug that is an oral lipid formulation of cidofovir and is less nephrotoxic. Our center has had positive experiences with the compassionate use of this agent. Polymerase Chain Reaction testing (PCR) is useful for diagnosis as it is highly sensitive and specific. Due to significant morbidity and mortality as well as limited data on prevention and treatment, it is important to consider adenovirus as a causative infectious agent in solid organ transplant patients who present with fever of unknown origin, pancytopenia and hemorrhagic cystitis. It is critical to rule out disseminated adenovirus disease, reduce immunosuppression where possible, and consider starting anti-viral therapy early. Brincidofovir is currently in phase three clinical trial for adenovirus infections.

Biography:
Sudhanshu Abhishek has evolved from his biotechnological skills and with post-graduation in Human Genetics, to understand the infectious disease-like, Tuberculosis (TB). During his mid-tenure of PhD thesis, he was selected for NIH-FOGARTY Fellowships (USA), to be trained on microarray technology at NYU School Medicine, NY, USA. His keen evaluation and interest to understand the host-pathogen interaction has opened new avenues of research in intraocular TB through the models (animal and cell line), with a goal to understand the pathogenesis and early diagnosis of intraocular TB, which may lead to better therapeutics. He has grown well from his 6 years of pre-doctoral training in this field through his continuous research, actively participating in teaching program of the department.
Abstract:
Statement of the Problem: Intraocular tuberculosis (IOTB), one of the extrapulmonary form of tuberculosis (TB), is a significant cause of inflammation and visual morbidity in TB endemic countries. Studies on IOTB are extremely challenging due to lack of appropriate human IOTB specimens, hence animal models of IOTB are required. Methodology & Theoretical Orientation: In the present study, a mouse model of IOTB was established by infecting the animals with Mycobacterium tuberculosis (M. tb; H37Rv) via intravenous (i.v.) route. Bacteriological evidence, histopathological changes and whole genome microarray study was done to identify the M. tb transcriptional signatures in mouse eye. Findings: At 45 days, post-infection (dpi), M. tb bacilli were observed in the eyes of 5 out of 12 (45%) M. tb challenged mice, whereas all the 12 animals showed positivity for M. tb RNA. Apart, histopathology of one CFU positive eye demonstrated intraretinal granuloma and moderate tissue damage in comparison to CFU negative eye that showed mild disease condition with no granuloma. Mycobacterium tuberculosis transcriptome analysis through microarray platform in the infected eyes, showed upregulation (≥ 1.5-fold) of 12 M. tb genes, where top three upregulated transcripts included Rv0962c, Rv2612, and Rv0984. Real-time validation of these top three genes showed an average of 7.40, 4.13 and 3.47 Log2 fold upregulation (p<0.05), respectively. Conclusion & Significance: Although, ocular bacterial load was low, but detection of M. tb RNA with undetectable tubercle bacilli in the animals confirmed the paucibacillary nature of IOTB developed under experimental conditions, similar to that observed in human IOTB patients. Upregulation of mycobacterial genes, suggest that the adaptation of M. tb in ocular environment, an immune-privileged site, may be associated with enhanced transcription of genes whose products are required for virulence and survival in intraocular environment. These genes/gene products could be important candidates for understanding the pathogenesis as well as development of new diagnostics/therapeutics for IOTB.
Horia Radid
National Institute of Hygiene, Morocco
Title: Microbiological quality evaluation of the commercialized raw cow’s milk in Salé

Biography:
Horia RADID possess laboratory experiments in the microbiology and genomic biology, medical, bacteriological and microbiological of food, water and food hygiene analysis. The objective of this work is to evaluate the microbiological quality of foods and food hygiene in order to raise the consumer awareness and to establish in the whole country a successful information system for the investigation and the monitoring of the diseases
Abstract:
Among the most popular origins of diseases that have relation with feeding, we find, the perishable commodities and particularly the milk and its products especially during the very hot summer days. The matched methods for conservation of milk and the hygiene measures had never been respected.
The objective of this study allows estimating the microbiological quality of raw cow’s milk of 120 taken samples, at Salé, from four farms, four peddlers and four dairies during spring 2013.In all the samples that we analyzed, we looked for many micro-organisms, like the total aerobic mesophilic flora, the total coliforms and fecal coliforms, Escherichia coli, Staphylococcus aureus, Streptococcus β-hemolyticus, listeria Monocytogenes, Salmonella and Brucella abortus. The synthesis of the obtained global results during the microbiological tests of the cow’s raw milk which is collected from farms, peddlers and dairies, doesn’t show any specific fluctuations during all the way long of the trial period. Indeed, it doesn’t matter if the raw milk has been collected from a farm, peddler or a dairy; the microbiological quality test is always the same whether it is qualitatively or quantitatively. It is then necessary to create some effective control measures, in order to protect the health of the consumer. For the best milk quality, the dairy farmers must submit the most efficient hygienic methods.
- Vaccines
Location: Paris, France
- Bacterial Susceptibility & Resistance
Location: Paris, France
- Laboratory Diagnosis of Infectious Diseases
Location: Paris, France
- Respiratory Diseases
Location: Paris, France
- Viral Infectious Diseases
Location: Paris, France
- Nosocomial Infections
Location: Paris, France
- Microbiology and Infectious Diseases
Location: Paris, France
- Infectious Diseases in Asia
Location: Paris, France
- Emerging Infectious Diseases
- Track 1:Ebola Outbreak and Approaches for Prevention
Track 2:Fungal Infectious Diseases
Track 3:Parasitic Diseases
Track 4:Public health practice
Track 5:Infectious Agents and the Human Immune Response
Track 6:Laboratory Diagnosis of Infectious Diseases
Track 7:Molecular Diagnostics of Infectious Diseases
Track 8:Infectious Diseases in Critical Care Medicine
Location: Paris, France
Session Introduction
Jamal Tazi
University of Montpellier, France
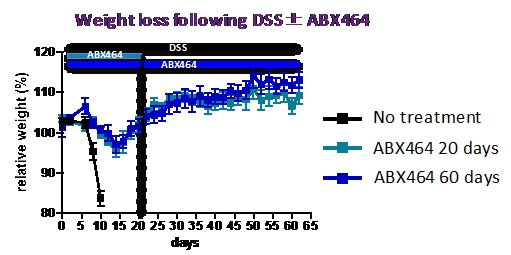
Title: The anti-hiv candidate abx464 dampens intestinal inflammation by triggering il22 production in activated macrophages

Biography:
Jamal Tazi is professor of functional genomics at the University of Montpellier and deputy director of the health center biology " Rabelais" responsible for education and training. For 20 years , he led the team " messenger RNA metabolism in metazoans " within the Institute for Molecular Genetics in Montpellier ( IGMM ) where he made important contributions to understand the fundamental mechanisms of the expression of our genes and editing of their products.These discoveries are used today in the medical field through the development of a new therapy based on the use of small molecules to fight against viral infections.To ensure the transition between basic and applied research, and also to support these innovative projects to clinical stage , Jamal founded in 2008 the company Splicos and established its partnership with public institutions as a cooperative laboratory where, he became the scientific Director
Abstract:
The progression of human immunodeficiency virus (HIV) is associated with mucosal damage in the gastrointestinal (GI) tract. This damage enables bacterial translocation from the gut and leads to subsequent inflammation. Dextran sulfate sodium (DSS-treatment) is an established animal model for experimental colitis that was recently shown to recapitulate the link between GI-tract damage and pathogenic features of SIV infection. The current study tested the protective properties of ABX464, a first-in-class anti-HIV drug candidate that has demonstrated anti-viral activity in HIV treatment of naïve patients. ABX464 also induced a long-lasting control of the viral load in HIV infected humanized mice after treatment arrest. ABX464 treatment strongly attenuated DSS-induced colitis in mice and produced a long-term protection against prolonged DSS-exposure after drug cessation. Consistently, ABX464 reduced the colonic production of the inflammatory cytokines IL-6 and TNFï¡ as well as that of the chemoattractant MCP-1. However, RNA profiling analysis revealed the capacity of ABX464 to induce the expression of IL-22, a cytokine involved in colitis tissue repair both in DSS-treated mice. A comprehensive analysis of the gene expression profiles by RNAseq demonstrated that the expression of IL22 was preferentially induced by ABX464 in mouse bone marrow derived macrophages only upon stimulation with LPS. Importantly, anti-IL22 antibodies abrogated the protective effect of ABX464 on colitis in DSS-treated mice.
Because reduced IL-22 production in the gut mucosa is an established factor of HIV and DSS-induced immunopathogenesis, our data suggest that the anti-inflammatory properties of ABX464 warrant exploration in both HIV and inflammatory ulcerative colitis (UC) disease.
Hailay Gesesew
Flinders University, Australia
Title: HIV care continuum outcomes: does Ethiopia meet the UNAIDS 90-90-90 targets?

Biography:
Hailay Gesesew has his expertise in Epidemiology. His multi-method approach assessing in each cascades of HIV care continuum will establish a significant contribution for the AIDS Ending goal. He has been publishing a lot of peer reviewed articles on the area of HIV care in reputable journals. Hiis publications produced from his PhD will improve the HIV care in developing countries especially Ethiopia. Hailay has been serving as a clinician, academician and researcher.
Abstract:
Background: How Ethiopia’s UNAIDS 90-90-90 targets is progressing was not assessed. We assessed HIV care continuum outcomes as surrogate markers for the 90-90-90 targets. Methodology: Data were collected from a 12 years retrospective cohort from anti-retroviral therapy (ART) clinic in Southwest Ethiopia. For measuring the UNAIDS diagnosis target, prevalence rate of delayed HIV diagnosis was considered as a surrogate marker. For the treatment target, number of people on ART, number of people who discontinued from ART or transferred out, and number of people who had fair or poor adherence were used as surrogate markers. For the viral suppression target, number of CD4 counts and/or WHO clinical stages were used to assess immunological, clinical and treatment successes and further show the viral suppression. Summary statistics, trends and estimated survival time were reported. Findings: 8172 patients were enrolled for HIV cares in 2003-2015. For the diagnosis target, 34.5% patients knew their status early (43%-children, 33%-adults). For the treatment target, 65% patients received ART, 1154 (21.9%) patients discontinued from ART, 1015 (19.3%) patients on ART transferred out to other sites, 916 (17%) of patients on ART had fair or good adherence. For the virological suppression target, 80.7, 80.3 and 65.8% of patients had immunological, clinical and treatment success displaying an estimated 66% of patients achieved the target. Conclusions: The finding reflects that an estimated 35% of patients knew their status timely, 65% of diagnosed patients received treatment and 66% of patients on ART achieved viral suppression. This is very far from the UNAIDS 90-90-90 targets underscoring the need for concreted efforts such as use of unmanned aerial systems (or drones) for transporting laboratory specimens, immediate or same day ART initiation, community distribution of ART, runaway packs during conflict, and use of GenXpert for HIV viral load testing would help to hit the target.
Harpal S. Mangat
Howard College of Medicine, Washington DC
Title: Correlation of Lyme disease with Immune Dysfunction

Biography:
Harpal S. Mangat, MD is in Practice in Maryland. He is an Assistant Professor at Howard University College of Medicine. He submitted recommendations to his US senator that got incorporated into the 2010 Affordable Health Care Act. He has four issued US patents and additional patents have been filed. He is a graduate of the Royal College of Surgeons Ireland, trained at Trinity College Dublin, Oxford University and London University in Family Practice and Ophthalmology. In the US, he trained at University of South Florida and Mercy Hospital Philadelphia in Ophthalmology and Internal Medicine. He is the transport physician for difficult cases returning to United Arab Emirates. His clinical interests include innovative new technologies, neuroprotection, diabetes, sleep apnea, Lyme disease, especially its neurological manifestations, as well as long distance air transport of seriously ill patients. He sees patients at his office in Clarksburg, MD (www.clarksburgmed.com) and Fredrick, MD.
Abstract:
Background: Lyme disease is caused by the bacterium Borrelia burgdorferi, transmitted to humans through the bite of infected blacklegged ticks. CD4/CD8 ratios in healthy adults vary across populations; in the US, a CD4/CD8 ratio ranging from 0.9 to 1.9 is considered to be normal in non-immunocompromised individuals. Lyme disease is diagnosed based on symptoms, physical findings (eg. Rash) and the possiblity of exposure to infected ticks. Labratory testing is helpful if used correctly and performed with validated methods. The US Center for Disease Control (CDC) diagnostic criteria requires the identification of five Western blot IgG bands for a positive diagnosis1, although patients with less than five positive bands have been subsequently diagnosed with Lyme Disease through urine PCR in Nanotrap testing2. Material/methods: 183 patients at two medical centers were evaluated in Lyme endemic communities in Maryland, US. Further investigation of 148 of these patients correlated their CD4/CD8 ratio with their Ig41 band, using one and two tail testing. Results: The mean CD4/CD8 ratio in the 148 patients was 2.41 with a variance of 1.05 and a standard deviation of 1.025. Assuming a normal CD4/CD8 ratio of less than 2, with a 5% confidence interval, the p value on both a one tailed and two tailed test was shown to be 0.00001. Two patients with an initial CD4/CD8 ratio of 2.7 and 2.8 who were IgG 41 positive were subsequently tested with the Nanotrap Urine PCR and found to be positive for Lyme. Conclusions: Increased CD4/CD8 ratio with a positive IgG 41 band appears to be a strong predictor of a subsequent diagnosis of Lyme disease despite current diagnostic guidelines. Further research should not only be directed towards investigating how Borrellia Burgdoferi disrupts immune function, but also towards improving diagnostic guidelines in light of validated diagnostic methods.

Mahmoud Magdi
Mansoura Faculty of Medicine, Egypt
Title: An epidemiological (field study) on Mansoura University Medical Students Determining Knowledge of Ebola virus outbreak.

Biography:
Mahmoud Magdi is an undergraduates in the Mansoura University, School of Medicine, Mansoura, Egypt. He was born in Fujairah, UAE, from full Egyptian parents, and later moved to the Egypt for higher Education. In 2014, He made the decision to pursue Medicine as a life career and was a member of Mansoura University Safety Society (MUSS). He aspires to seek higher education and health care profession in other continents such as Europe and North America. Because of his love for research, he continues to strive for the needs of international students by leading the Mansoura University Safety Society from 2016. He also plans to continue making research in the future regarding the implementation and improvement of health care.
Abstract:
Sindew Mekasha Feleke
Ethiopian Public Health Institute, Ethiopia
Title: Evidence for possible interruption of onchocerciasis transmission in metema focus, north gondar, ethiopia

Biography:
Abstract:
Background: Onchocerciasis is a neglected tropical parasitic disease (NTD) caused by a filarial nematode worm called onchocerca volvulus and transmitted by the bites of simulium flies. Since 2001, Ethiopia has been committed to implementation of the National Onchocerciasis Control Programme, which was revised during 2012 to undertake elimination through interruption of transmission until 2020. This strategy uses annual or semiannual community-based treatment using the drug Ivermectin.
Objective: This study was aimed at assessing whether the goal of focal transmission interruption attained or not in one of the areas receiving annual community based Ivermectin for more than a decade.
Methods: A community-based cross sectional study was conducted in selected communities of Metema focus during 2014 and 2015 in North Gondar, Ethiopia. High endemicity before intervention, proximity to the breeding sites and representativeness of the focus within 20-30 km distance between sites was used for selection. The study participants were community residents above the age of 5 years for skin microfilariae survey and children’s born during the period of mass treatment with age below 10 years for Ov-16 IgG4 antibody exposure test. Skinsnip sample collected from left and right iliac crest of 2,986 individuals with sterilized biopsy punch and examined under a microscope after 24 hours’ incubation. Whereas, finger prick samples collected from 3,136 children and dried blood spot (DBS) prepared for Ov-16 ELISA laboratory analysis.
Results: From microscopic examination, no skin snip found positive for microfilaria. ELISA showed 0.25% (8 of 3,136) antibody positive. But molecular assay of skin snip using PCR demonstrated no infective parasite for those 8 sero-reactive children.
Conclusion: The skin microfilarial survey results revealed absence of Onchocerca volvulus in the community and the serology results implied that children born during the period of the intervention are protected from acquiring infection. An entomological assessment appears important to confirm absence of infectious flies in the focus and interruption of focal transmission.

Biography:
Abstract:
[Background and Aims] Although there are some cases complicated by toxic shock syndrome (TSS) from wound infections in extensive severe burns patients, they are rare case causing TSS in small range burn in adults.
For the patients suffering from small burn injuries, an intensive care is not usually needed for the primary care, as they admit in the general ward on admission day. However in rare cases these patients’ condition could get worse while having a treatment in the general ward, and they can be forced to move to the ICU until the vital sign gets stable. In this time, it was examined the TSS complicated by small range burn patients in adults. I report these rare cases with some our considerations.
[Methods] I have experienced 5 cases were complicated by TSS at some reason in inpatient treatment in burns to five years from January 2010 to December 2015, two cases are males and three cases are females, 24 years of age to 75 years (average 48.2 years). Of each case TBSA, PBI, sudden change time, outcome were examined .
[Results] TBSA is 3-32 (average 11.2). PBI is 26-76 (average 53.8), sudden change timing injury 4th to 14th or postoperative 1st to 13th, outcome 1 cases in five cases have been died
[Conclusions] Burn patients have low TBSA and PBI, there is a possibility that even easily getting worse. Particularly when complicated by infection, was easily considered caution because they may follow irreversible course when complicated by TSS. We suggest not to hesitate to move the patients to the ICU as soon and suggest that the teamwork and cooperation of the plastic surgery department and the ICU department are required.
Ayinalem Alemu
Ethiopian Public Health Institute, Ethiopia
Title: Status of Xpert MTB/RIF Assay Implementation in Ethiopia

Biography:
Abstract:
Background: In 2010, WHO has endorsed Xpert MTB/RIF Assay for the diagnosis of tuberculosis (TB) and rifampicin resistance tuberculosis (RR-TB). Following this recommendation, Xpert MTB/RIF Assay has been implemented in Ethiopia since 2012. Monitoring and evaluation of Xpert MTB/RIF Assay implementation is necessary to ensure the effective and efficient use of resources and to guide the future scale-up.
Objective: To assess the implementation Xpert MTB/RIF for the diagnosis of TB and RR-TB in Ethiopia.
Methodology: Data was collected and analyzed from 87 GeneXpert sites from May to June 2016. A structured questionnaire was used to collect information on staff profile and trainings taken. Data was extracted from GeneXpert machine since the date of installation from 70 GeneXpert sites. Records were reviewed from laboratory register book and from archived laboratory request formats by using a comprehensive assessment tool to evaluate the laboratory personnel competency and clinician’s adherence to the national algorithm.
Result: A total of 80,683 specimens were examined by using Xpert MTB/RIF Assay starting from the date of installation up to June 2016 in 70 GeneXpert sites. Mycobacterium tuberculosis was detected in 12,422 (15.4%) of specimens. From all TB detected results 83.75% (10,403), 12.68% (1,591) and 3.45% (428) were susceptible, resistance and indeterminate to Rifampicin respectively. The error rate was 14.1%. There were 285 Xpert MTB/RIF Assay trained laboratory professionals at 87 GeneXpert sites. An average of 3 trained laboratory professionals were working in each facility. At least one trained laboratory professional was found in each facility, but untrained laboratory professionals were performing Xpert MTB/RIF Assay in 67 facilities. National Tuberculosis Program approved Xpert MTB/RIF Assay testing algorithm was not followed in 36% of sites. Most of the clinicians did not properly fill request papers. Standardized request formats and laboratory log books were not available in 15% and 8% of facilities, respectively. Xpert MTB/RIF Assay results were correctly recorded on the laboratory log book in 87% of sites. Critical result (RR-TB) communication was not appropriate in 25.6% of facilities. Xpert MTB/RIF Assay test results were not archived regularly in 47% of laboratories.
Conclusion: Detection rate of TB with the Xpert MTB/RIF Assay was low. This may be due to inappropriate eligibility screening of the patients. Xpert MTB/RIF Assay showed an advantage for detecting RR-TB cases in peripheral laboratory level, which is important for early detection of drug resistant cases as well as early treatment initiation. Error rate was high in comparing with the expected standard (≤3%). There was 100% Xpert MTB/RIF Assay training coverage; however, in majority of the sites untrained laboratory professionals were performing Xpert MTB/RIF testing. This may probably have negative impact on test results.
Neeraj Chhari
Peoples college of medical science & research Center, India
Title: Diabetes: An Encroached Danger:A study from central India

Biography:
Dr.Neeraj Chhari 34 years is an assistant professor in department of community medicine in Peoples college of medical science & research Centre,Bhopal,India.He has done his MBBS(2008) MD(2012).He has done his”Certificate course in evidence Based Diabetes Management”(CCEBDM) in 2016 which is recognized by Public Health foundation of India(PHFI) & International diabetes Federation(IDF).He is life member of Indian association Preventive & Social Medicine(IAPSM) and World Non communicable disease(WNCD) federation.Dr.Neeraj is basically inclined towards non communicable diseases esp. diabetes and cancer. At his clinic since 2014 he has organized 4 diabetic camps till date .
Abstract:
INTRODUCTION: As the WHO report the Diabetes epidemic is more pronounced in India than anywhere else. Glycated hemoglobin is a form of hemoglobin that is measured primarily to identify the three-month average plasma glucose concentration. The test is limited to a three-month average because the lifespan of a red blood cell is four months (120 days). But RBCs do not all undergo lysis at the same time, so HbA1C is taken as a limited measure of 3 months.OBJECTIVES:To study the level of A1C level in Diabetic and Non diabetic patients in the suburban area to give recommendations on that basis METHODOLOGY: Cross sectional study was done on the patients coming to clinic during Diabetic camp organized in suburban area of city. RESULTS:Out of 143 T2DM patients the 112(78%) have HBA1C level within the range of 7-9%.Only 7(4.9%) patients have level >11%.37 patients out of 78 who were non diabetic has Hba1c level of more than 6.5%.CONCLUSION:The observational study was conducted in diabetic camp and it was observed that diabetes has encroached the society with large spectrum and Life style modification is needed to prevent.

Biography:
Sumedha Sharma started her research career with her dissertation in the postgraduate degree where she worked on the effect of Ocimum gratissimum on the colon cancer. She qualified various national eligibility test (Indian Council of Medical Research & Council of Scientific & Industrial Research, India) to pursue her goal in research and academics. Her inclination towards research lead her to join the doctorate program where her research was focused on tuberculosis (TB). During her doctorate degree, she was selected as a training participant in AIDS and TB international training and research program (AITRP) sponsored by Fogarty International Centre, NIH, USA where she was trained on microarray technology. Her microarray work on sputum of PTB patients gave an insight to the mycobacterial genome specifically expressed in active TB patients, leading to identification of mycobacterial targets, which can be exploit as potential vaccine and diagnostic candidates.
Abstract:
Statement of the Problem: Tuberculosis (TB) diagnosis is a one of the major areas of interest to control the spread of TB disease in community. Therefore, there is a need to develop rapid and specific diagnostics easily usable at different health care levels. Our previous work on mycobacterial gene expression pattern in sputum from pulmonary tuberculosis patients lead to identification of newer targets, as potential biomarkers. In view of this, the current study was planned to evaluate the role of these candidate biomarkers in molecular and serodiagnostic tests. Methodology: Three of the genes, Rv0986 & Rv0971 along with one Region of Difference (RD) gene Rv3121, were evaluated for their diagnostic potential in RNA based real time (RT) polymerase chain reaction (PCR). Simultaneously, the peptides from proteins corresponding to these genes along with five other RD genes were evaluated for their serodiagnostic potential using a peptide based enzyme linked immunosorbent assay (ELISA) technique. Findings: The use of the target genes Rv0986, Rv0971 and Rv3121 in a molecular RNA based assay lead to the detection of smear positive patients with 100%, 87% and 94% sensitivity and of smear negative TB patients with 50%, 58% and 67% respectively. However, of all the peptides corresponding to different proteins which were tested in the serodiagnostic ELISA the maximum sensitivity that could be attained was 37% for smear positive PTB patients and 32% for smear negative PTB patients. Conclusion & Significance: A subset of the proteins encoded by the genes expressed by mycobacteria in the sputum have shown less sensitivity for the development of a serodiagnostic assay, but these genes have shown promising results for the development of a RNA based molecular assay that can be optimized further after evaluation in a larger cohort of patients.
Seddiki Sidi Mohammed Lahbib
University center of Naâma, Algeria
Title: Nosocomial Fungal Infectivities of In Vivo Candida Biofilms

Biography:
S.M.L. Seddiki is a lecturer at University Center of Naama. He had these degrees of undergraduate and graduate at the University of Tlemcen - Algeria. Seddiki’s research contributes to the struggle against fungal nosocomial infections, particularly those caused by Candida sp, he proposed the term: INFECTIVITY to distinguish fungal infections from simple contamination
Abstract:
Invasive nosocomial infections due to Candida species are responsible for increasing the length of stay, cost of hospitalization and morbidity in immunocompromised patients. Their severity and rapid progressivity are owed to the difficulty of diagnosis. Various catheters, which are often used to train a body fluid (blood, urine, infusion, parenteral nutrition, medication ...) inside the body of the patient or vice versa, are susceptible to be altered by Candida sp. and promote the formation of biofilms which consolidates the risk of invasive nosocomial infections; i.e., these structures are considered as a nest for disease because it is not easily eradicate by conventional antifungal therapy. Such as the diagnosis of candidiasis related to catheter is difficult, the differentiation between catheter infection and a simple contamination is essential to establish an antifungal treatment. Our study aimed adapts to yeasts the Brun-Buisson (1987) method which only concerned by bacteria, it’s why we conducted our study between February 2011 and January 2012 at the Hospital University Center of Sidi Bel Abbès-Algeria that aims to evaluate the various types of fungal catheters infectivities (contaminations, colonization and infections) and their corresponding rates, as well as the responsible yeast species. At the end, the ability to form biofilms was checked. The results showed that three types of fungal infectivities of catheters were identified. On the other hand, SEM images showed clearly Candida biofilms on the surfaces of catheters.

Biography:
Abstract:
Antimicrobial resistance (AMR) is a growing public health concern worldwide and is one of the top health challenges facing humanity in the 21st century. AMR among enterobacteriaceae is rapidly increasing especially to third-generation cephalosporins and carbapenems. Further, strains carrying mobilized colistin resistance (mcr) genes 1 & 2 have been isolated from humans, food-producing animals, and environment. Uncontrolled use of antibiotics in animals in large scale could be one of the major contributing factors to generation and spread of antibiotic resistance. No studies have been done to evaluate antimicrobial resistance in animals in Qatar. This study aimed at establishing a primary baseline data for prevalence of antimicrobial resistance among food animals in Qatar. 172 fecal samples were obtained from two broiler farms andone live bird market in Qatar and 90 Escherichia coli (E. coli) bacteria were isolated and subjected to antimicrobial susceptibility testing using Etest method. 90% (81/90) of the isolates were resistant to at least one of the 16 tested antibiotics. 15.5% (14/90) of the isolates were colistin resistant, 2.2% (2/90) were extended spectrum β lactamase (ESBL) producers and similar percentage were multi-drug resistant (MDR) to four antibiotic classes. ESBL-producing E. coli and colistin resistant isolates were confirmed using double disc susceptibility testing and PCR, respectively. In Summary, Our results indicates high antimicrobial resistance in food producing animals in Qatar, including ESBL and colistin resistance. Such AMR bacteria could be easily transmitted to humans through consumption of undercooked food or noncompliance with hygiene practices, which mandates prompt development and implementation of stewardship program to control and monitor the use of antimicrobial agents in community and agriculture.
- Parasitic Diseases | Vaccines
Session Introduction
Lara Ricotta
Statens Serum Institut, Copenhagen, Denmark
Title: Comparison of screening method and cohort design to estimate pertussis vaccine effectiveness in Denmark, 2000-2014.
Biography:
Abstract:
Sindew Mekasha Feleke
Ethiopian Public Health Institute (EPHI), Addis Ababa, Ethiopia
Title: Sero characterization of Plasmodium species in Limu Kossa District of Jimma Zone, Western Ethiopia
Biography:
Sindew Mekasha Feleke, born on Feb-04-1985 and Employed in Ethiopian Public Health Institute in 2007 GC. He had did his Biology (BSc) from Dilla University , Tropical and Infectious Disease (MSc) from Addis Ababa University, Guest Researcher Fellowship at CDC lab Atlanta, USA for one and half months, Guest Researcher Fellowship at University of South Florida (USF) lab, USA for two months
And he had more than Nine (9) years work experience at the Ethiopian Public Health Institute (EPHI) since 2007 GC until know. Currently he is working as an Malaria and Neglected tropical Diseases Team Leader, Head for Malaria RDT QA and Onchocerciasis Molecular Laboratory and Researcher 1
Abstract:
Aiman El-Saed
King Abdulaziz Medical City, Saudi Arabia
Title: Benchmarking of healthcare-Associated infections in Gulf Cooperation Council (GCC) states
Biography:
Dr Aiman El-Saed is MD physician from Egypt who had PhD and MPH in epidemiology from the University of Pittsburgh, Pennsylvania, USA in 2004. Worked as a researcher at the University of Pittsburgh for 3 years between 2004 and 2007. Currently working as Assistant Professor of Epidemiology & Biostatistics at the College of Public Health and Health Informatics of King Saud bin Abdulaziz University for Health Sciences (Riyadh, Saudi Arabia). He is also working as advisor of health surveillance at the infection Prevention & Control Department, National Guard hospital, Riyadh, Saudi Arabia. He is serving as primary or co-investigator of several research grants. He had a strong epidemiologic and statistical research experience.